Abstract
Multicenter large collaborative research groups have been the cornerstone for advances that have been made in multiple disciplines in medicine. These collaborative groups are specifically useful in situation where no single center based dataset is large enough to effectively address biological and clinical relevant questions that could advance the field. Most such collaborative groups exist in the developed countries and have contributed significantly to the development of the current standards of care in leukemia. The challenges in the developing countries or low middle income countries (LMIC) are distinctly different and often algorithms that have evolved in the developed world may not be applicable, relevant or accessible in the LMIC. It is imperative that these challenges be addressed through large multicenter studies that are located within the LMIC and appropriate local data driven solutions be implemented in response. The 'Hematological Cancer Consortium' is a collaborative group from India currently compromising twelve institutions spread across the country that have come together to collaborate in the field of leukemia. As an initial exercise, to establish denominators a retrospective data analysis was undertaken (Indian acute leukemia research database [INwARD]). Here we present the retrospective analysis of the acute myeloid leukemia (AML) data.
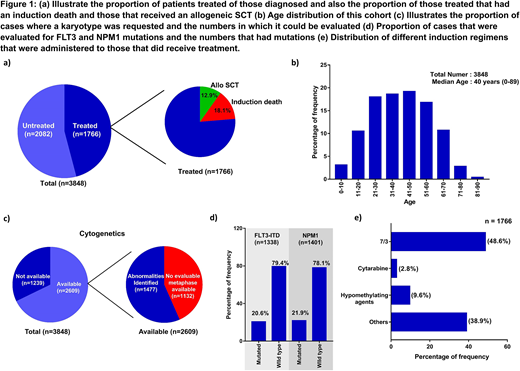
Retrospective data from January 2013 to December 2017 was collected from 10 large tertiary centers from across the country (in one center data was available only from January 2017). A central online data capture and management system was in place which was independent of all the participating centers (Clinical Data Management Center [CDMC], Vellore, which is compliant with standard ICH-GCP regulations). In this initial phase some centers contributed data offline to the data management center. A total of 3848 were confirmed to have had a diagnosis of AML in this period of which it was noted that 1766 (46%) received definitive treatment (Fig 1 a). The median age of the patients was 40 years (range: 0-89) and there were 59% males. The age distribution of patients by each decade is illustrated in Fig 1b. 399 (10.4%) were ≤ 18 years). A sample for karyotyping was sent in 2609 (68%) however of these an evaluable karyotype was noted in only 1477 (57%) (Fig 1c), the reasons for lack of evaluable metaphases was not clear. A FLT3 and NPM1 mutation status was evaluated in 1338 (35%) and 1401 (36%) respectively. Of the evaluated patients 20.6% and 21.9% had FLT3-ITD and NPM1 mutated respectively (Fig 1d). Of the 1766 patients that were treated 858 (48.6%) received a conventional 7/3 induction, 170 (9.6%) received hypo-methylating agents while the rest received various abbreviated dose regimens and a small proportion (2.8%) received high dose cytosine based regimens as induction therapy. Antifungal prophylaxis was used by 82% of patients that received therapy. Of those that received induction therapy there were 18% induction deaths and 12.9% subsequently received an allogeneic SCT as part of their consolidation therapy (Fig 1a). The 5 year KM estimate for overall and event free survival for the patient that received treatment was 56.2±2.6% and 33.8±2.4% respectively.
The data illustrates significant challenges and opportunities with the management of AML in India. A significant proportion of cases do not receive definitive therapy nor do they have conventional tests such as karyotyping or molecular tests done as part of the baseline diagnostic tests, various social and financial constraints could contribute to these and these need to be evaluated in more detail. Strategies to increase access to care and laboratory facilities along with an effort to reduce early induction deaths need relatively urgent attention. The relatively young age of the cohort and large number of cases would allow us to address relevant biological and clinically challenges effectively, in the future, in this cooperative setting.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal